As a medical translator with a background in nursing, I was delighted when my son Leo chose to train as an emergency medical technician (EMT) and join the Madrid ambulance service. He’s shown me round various ambulances and we often chat about trauma, technology and terminology. This March, I got the opportunity to find out how his experiences, and the terms he and his colleagues use, differ from their counterparts in the UK. I stepped on board a UK ambulance for a guided tour by my friend Jon Murrell, a paramedic practitioner stationed at Redhill, in Surrey. We spent the afternoon packing and unpacking equipment, locking and unlocking drug storage systems, opening and closing carry chairs and other transfer devices, and over a coffee we thrashed out the pros and cons of English and Spanish ambulance crew training, logistics and communications.
This article was first published in the May-June 2022 issue of the ITI Bulletin in a slightly shortened form. For reasons of space and readership demographics, I omitted some technical details and focused more on linguistic aspects. Here is the full 2500-word version.
Table of contents
- Past and present
- Crews and qualifications
- The three Rs
- Emergency apps
- Logistics
- Equipment
- ABC
- Names, terms and pronunciation
- PPE
- Recognition on the road and at the scene
- References
Past and present
Ambulances have changed radically in the past half-century, from 1970s vehicles carrying the bare minimum – stretcher, splints and oxygen – to today’s medicalised ambulances providing advanced life support. State-of-the-art equipment needs skilled hands, so crew qualifications and training have developed in parallel.

Historically, the UK ambulance system has followed the ‘take-the-patient-to-hospital’ model (modelo parasanitario), where paramedics give emergency care and blue-light patients to hospital,1 while Spain adopted the European ‘take-the-hospital-to-the-patient’ model (modelo médico extrahospitalario),2 where doctors and nurses provide advanced on-the-scene medical services. With today’s highly qualified paramedics, the UK system has morphed into a hybrid clinical model (modelo paramédico).
So who does what and where? Levels of care, crew roles and logistics vary from one region to another in both countries. For this article, I’m focusing on advanced ambulances only and excluding basic life support services for low-acuity incidents, non-emergency patient transfer services – affectionately known as ‘granny runs’ – (traslados programados) and event cover (preventivos). And I’m referring specifically to SECAmba in the UK and the Madrid ambulance services in Spain. To complicate matters, Madrid quirkily breaks down emergency care by place delivered: SAMURb responds to calls in public places and SUMMAc at patients’ homes.
a SECamb: South East Coast Ambulance Service b SAMUR: Servicio de Asistencia Municipal de Urgencia y Rescate - Protección Civil (Municipal Emergency Care and Rescue Service - Civil Protection) c SUMMA: Servicio de Urgencias Médicas de Madrid (Madrid Medical Emergency Service)
Crews and qualifications
Each UK ambulance is double-crewed with combinations of paramedics, associate ambulance practitioners (AAPs) and emergency care support workers (ECSWs), all of whom hold a C1 driving licence. Paramedics are the most senior. With a BSc degree – and a master’s in the case of paramedic practitioners – they’re trained to intubate, cannulate, resuscitate, and perform other techniques not ending in -ate. Second up are AAPs – known as EMTs in other regions. After an 18-month apprenticeship, they can give intramuscular injections, splint patients and even deliver babies. Finally, ECSWs receive a three-month induction and are ready to defibrillate hearts, dress wounds, take a set of ‘obs’ (temperature, pulse and blood pressure) and move patients safely. Confusingly, ECSWs are known by a plethora of names across the 11 ambulance trusts in the UK: ambulance care assistants, ambulance care attendants, clinical care assistants, emergency ambulance crew and emergency care assistants.
By contrast, Spanish ambulances have a crew of two to four people, with a combination of doctor and/or nurse, and one or two EMTs. In Madrid, ambulance doctors and nurses hold a master’s in out-of-hospital emergency medicine.3 The course to train as an EMT (TES, técnico en emergencias sanitarias) in Spain is longer and more classroom-based than its counterpart in the UK. EMTs drive the ambulance and work alongside the doctor and nurse. Their skills vary considerably, according to the ambulance service concerned.
The three Rs
The right care at the right time in the right place
“Emergency. Which service?”
In the UK, if you dial 999 (or 112 or 911) for an ambulance, you’ll be put through to an emergency medical advisor who triages the call via the NHS Pathways system,4 with paramedics and nurses on hand to advise if needed. Some 10% of calls are resolved on the spot (Hear & Treat – refer or discharge); otherwise, an ambulance is dispatched and reaches the patient in an average of 7, 18, 120 or 180 minutes,5 depending on the level of acuity (life-threatening, emergency, urgent, less urgent). Some emergencies are resolved at the scene (See & Treat – refer or discharge), but 60% of all calls end up with a patient in hospital (See & Treat – convey).
“¿Dónde está? ¿Cuál es su emergencia?”
In Madrid, if you dial 112 (or 911) for an ambulance from a public location, you’ll be put through to an EMT in SAMUR, who triages the emergency following an automated pathway (árbol de decisiones) and dispatches a basic or advanced ambulance for every single call received. Surprisingly, SAMUR doesn’t have access to your medical record at the call centre or on the ambulance. If you phone from home, a doctor in SUMMA takes the call, gives advice (consejo médico) and solves the problem (resolución telefónica), or dispatches the appropriate vehicle crew (dispositivo) – a rapid-response vehicle, advanced ambulance or a home-care unit. Happily, SUMMA can access your medical record. These idiosyncratic systems work efficiently, however, matching the UK response times in like-for-like categories (emergencia, urgencia no demorable, urgencia demorable, aviso domicilario).
Paramedic practitioners in the UK also sometimes attend emergencies in a single-response vehicle that has room to assess a seated patient in the back but not to transfer the patient to hospital. Similarly, in Madrid, a SUMMA crew may be dispatched in a fast-response vehicle (vehículo de intervención rápida) to attend patients while waiting for ambulance back-up.


Emergency apps
Even a fast seven-minute ambulance response time may be too long for someone in cardiac arrest. But there’s an app for that. In the UK and Spain, emergency healthcare professionals voluntarily register with GoodSAM and My112, respectively, and the app pings them when they’re in the vicinity, marking the precise location of the incident and nearest defibrillator (DEA). Madrid goes one step further with its CardioMAD app, instructing a bus driver to pull up at the next stop while pinging a volunteer to collect the defib from the bus and rush it to the scene.

Logistics
A UK ambulance carries sufficient spares for a 12-hour shift, although some shifts may be shorter. After completing a job, the crew does a quick clean-down, books clear with the operations centre, and is dispatched elsewhere. No rest, no restocking. If spares run out, say, from using two maternity packs in quick succession, the crew returns to base to do a hot load or even switch to a freshly prepared ambulance. At the base, outsourced workers, known as vehicle preparation operatives, deep-clean, restock and refuel the ambulances round the clock. By contrast, Spanish crews work 12- or 24-hour shifts, and if there’s time between calls, they return to base to clean, restock and even rest or sleep.
Equipment
Splints, stretchers and oxygen have come a long way in the past few decades. Ambulance crews in the UK and Spain now have access to a wide range of devices, from vacuum splints (férulas de vacío) to Frac-Straps™, scoop stretchers (camillas cuchara) and carry chairs (sillas plegables). Oxygen cylinders (balas de oxígeno) have evolved too, from steel and then aluminium, to today’s lightweight carbon-fibre casing.
Essential supplies must be easily accessible, so UK paramedics grab a fully equipped primary response bag as they jump off the ambulance, with drugs stored in brightly coloured pouches, and intravenous morphine and diazepam securely fastened to their belts. Spanish kit is organised in circulatory and respiratory rucksacks, with drugs stacked on the ambulance in clearly labelled racks. The drug cabinets are kept unlocked because the vehicle is always left on run lock (engine on, doors locked) to keep devices powered up and drugs secure.


ABC
The ABC (airway, breathing, circulation) of resuscitation is the same wherever you are, so emergency equipment is common to all ambulances. Below is a list of some of the devices that Jon and Leo showed me on their ambulances. Each item starts with the descriptive term, followed in parentheses with the English and Spanish jargon that Jon and Leo use, respectively. Interestingly, abbreviations are often used in spoken English, brand names in Spanish and generic names in both languages. I’ve also added a few notes for some of the devices.
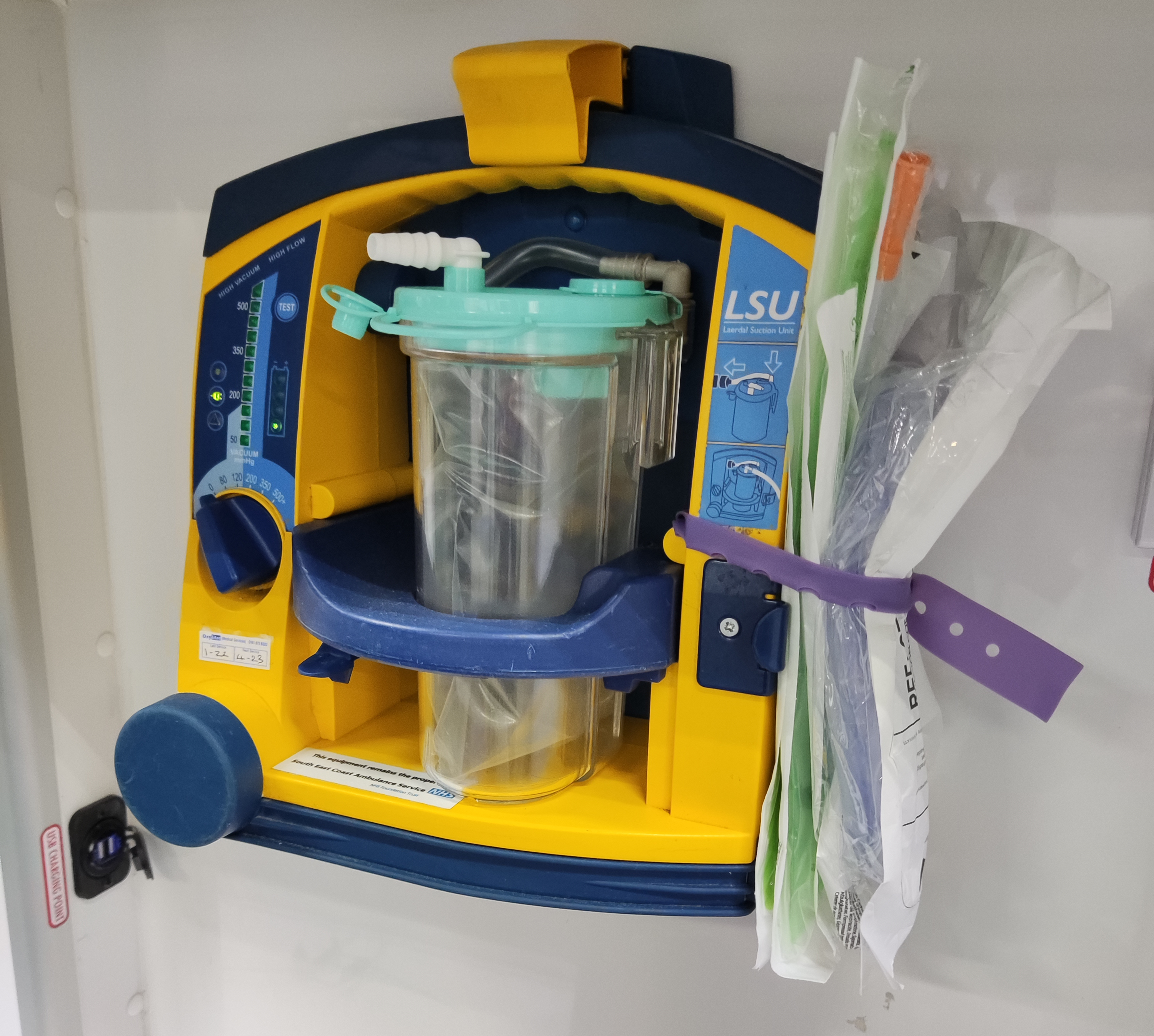
| Airway ● Portable oral suction kit (LSU; aspirador) |
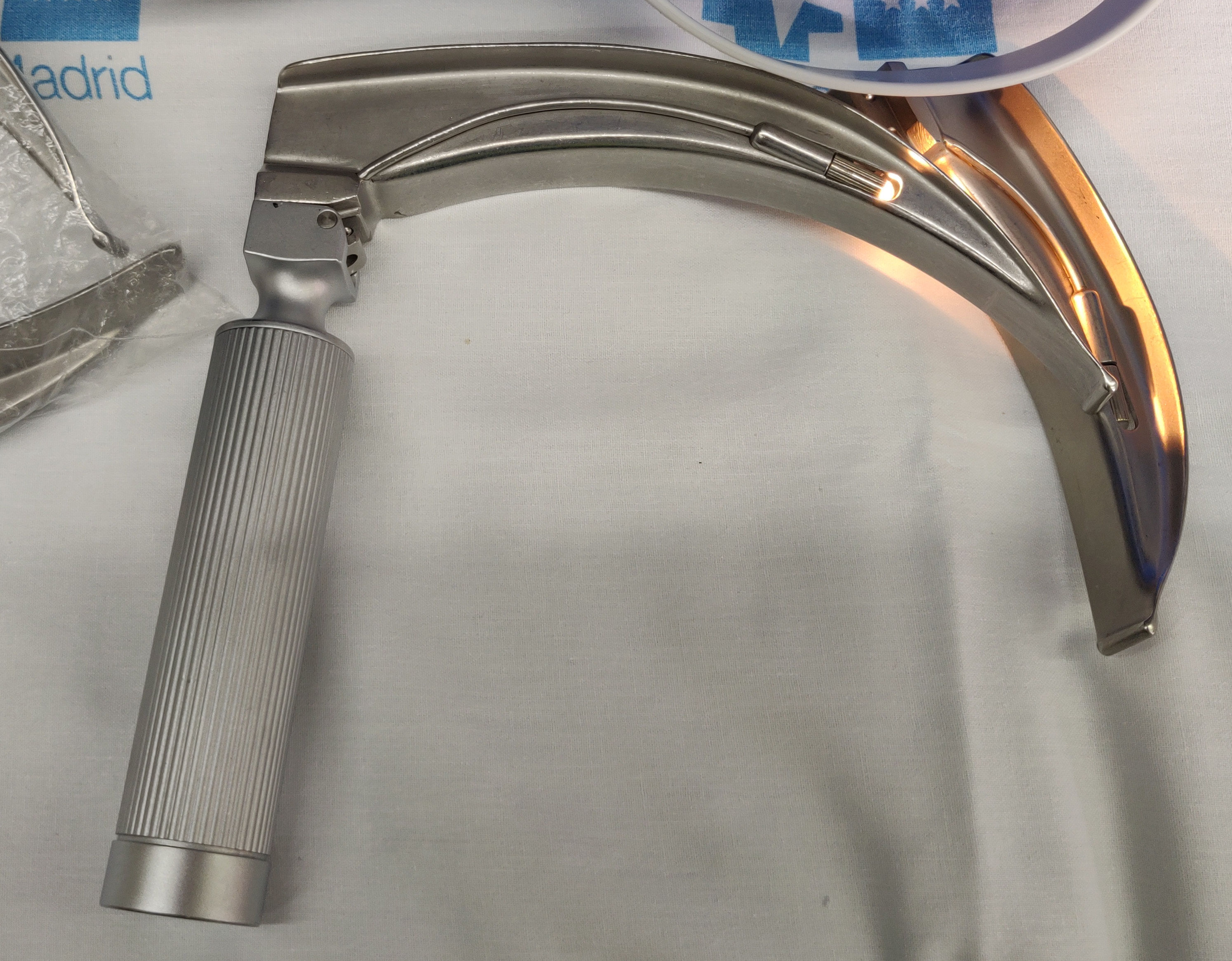
| Breathing ● Oropharyngeal airway (OP airway; Guedel™) ● Self-inflating bag-valve mask (BVM; Ambú™) ● Laryngeal mask airway (i-gel™; Fastrach™) – a supraglottic device inserted without a laryngoscope by AAPs and EMTs to secure and maintain an airway and for difficult intubations ● Laryngoscope (laryngoscope; laringo) ● Endotracheal tubes (ET tube; tubo endotraqueal) and introducers (bougie; Frova™ con fiador) – for intubations by paramedics and doctors ● Handheld ventilator (pollito) – a device used in Spain to replace manual ventilation in tight spaces like a lift ● Portable ventilator (Parapac™; respirador or Oxylog™) |
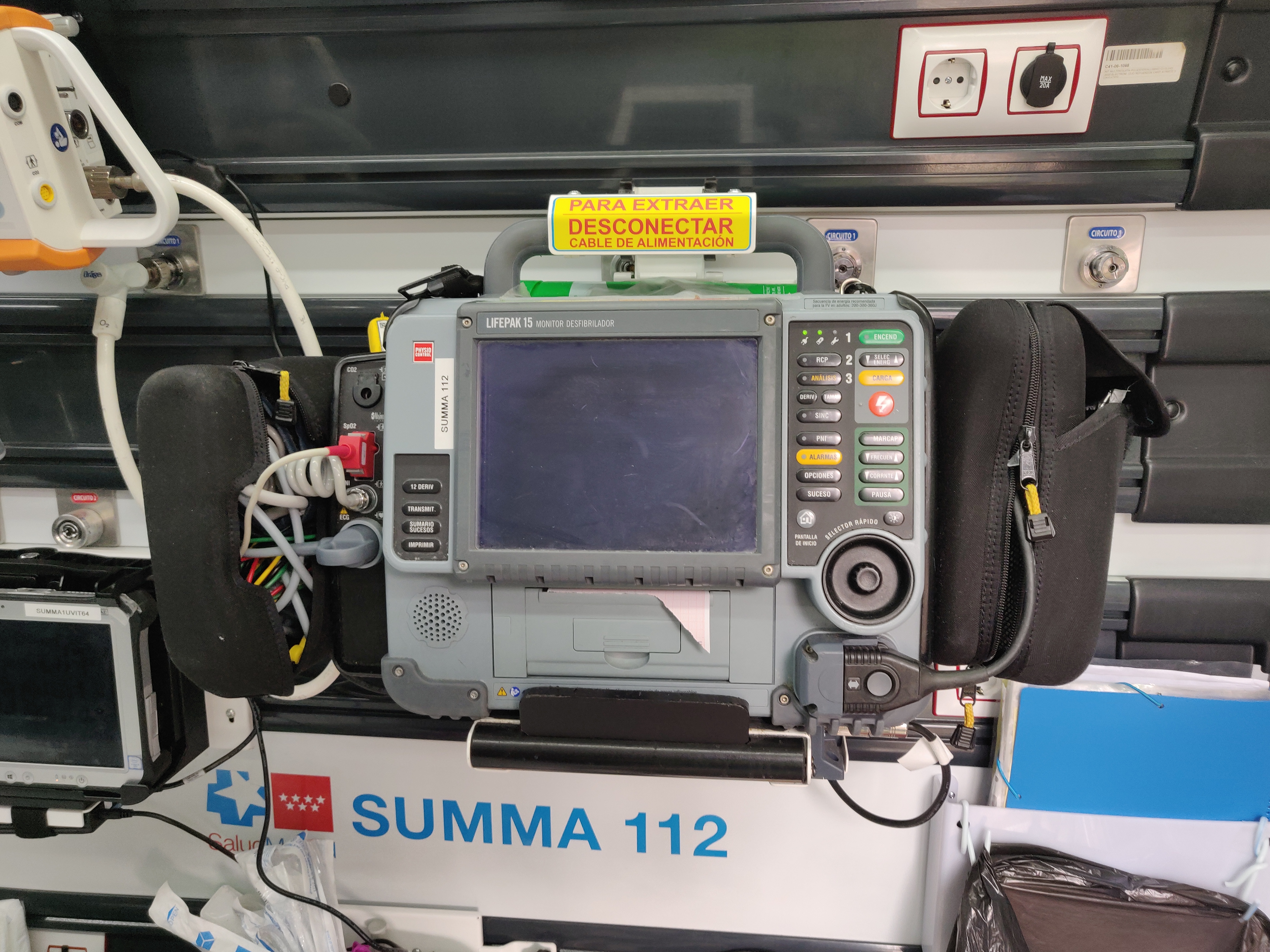
| Circulation ● Portable AED (defib; DAE) – first-on-scene defib and simple 3-lead ECG monitoring ● Monitor-defibrillator (Lifepak™ in both languages) – this is the ambulance centrepiece for manual or automated defib, 12-lead ECG, BP, pulse, temp, SpO2 monitoring, and EtCO2 reading to check airway placement. Data can be sent by Bluetooth to the ambulance tablet and from there to the patient’s centralised medical record. ● Chest compression system (Lucas™ in both languages) – mechanical cardiopulmonary resuscitation by means of a suction cup and apparatus. Used when manual CPR is unviable because of crew unavailability, exhaustion or when transferring a patient from the incident scene to the ambulance (evacuación primaria). |
Names, terms and pronunciation

Top: Spanish chick; Bottom: English turkey baster
Words spelled the same in English and Spanish can be pronounced quite differently, depending which syllable is stressed. Take the Ambu™ bag-valve mask, for instance, pronounced ˈambjʊ in English and amˈbu in Spanish. When other languages come into the mix, as in the case of the intubation guide called a bougie, it’s no surprise that pronunciation differs, with the English ˈbuːʤi resembling the French original more than the Spanish ˈbuːɡi with a hard g.
Device manufacturers love coining catchy names – Oxylog™, Frac-Straps™, i-gel™ – that soon become jargon. Sometimes crewmates come up with fun names themselves, so in Spanish, a small yellow handheld device (a Pneupac™ ventilator) is nicknamed pollito (chick), while in English the Suction-Easy™ aspirator shaped like a turkey baster is referred to as – you’ve guessed it – the turkey baster.
PPE
Personal Protective Equipment (PPE) in COVID times
Donning and doffing
In pre-COVID days, UK crews just put on gloves for clinical procedures. Now, they wear gloves, fluid-repellent surgical mask and apron (level 2 PPE) and ask patients to wear a face covering. If a patient has confirmed or suspected COVID, crew members up their PPE to level 3, donning coveralls, air-powered hood and gloves, and doffing in the opposite order.
Vestido y desvestido
In Spain, ambulance crews already lived in gloves. Now, in SAMUR6 they also put on FFP2 masks and goggles, and insist that patients wear a surgical mask. When attending patients indoors, crew members don a gown (bata) and goggles (protección ocular) when performing respiratory procedures. Level 3 PPE (capucha autoventilada y buzo) is optional when attending COVID-positive patients.
Recognition on the road and at the scene
Most ambulances share the same distinctive livery, with green-and-yellow Battenberg markings along the sides, chevrons at the rear and a blue Star of Life. However, English ambulances fill side panel space with awareness campaigns, ranging from a mnemonic for symptoms of sepsis to a dissuasive You wouldn’t call the coastguard if you fell in a puddle. Think before you dial! Spanish ambulance panels are less entertaining, simply displaying the emergency number and the regional service name. Interestingly, blue lights in Spain have only been blue quite recently; they were yellow until 2018.


Right: SUMMA ambulance and Leo Reyes
The crew uniforms are very different too – with a knock-on effect for how the crews communicate with patients and families. UK crews dress in sober green, with their job titles and pips displayed discreetly on epaulettes, making it hard for lay people to tell who’s who. Conversely, Spanish crews sport bright, high-vis garments with huge-lettered job titles across their backs – easy for everyone to read and understand. However, UK crew members have their first names sewn onto uniforms to encourage friendly communication with patients, while in Spain, patients often never learn clinicians’ names – badges on lanyards get tucked into pockets, clear of cables and tubes.
Names matter in verbal communication, too. UK paramedics will sound out how a patient wishes to be addressed, saying: “Hello, I’m Jon. What’s your name?”, and patients very rarely respond with a blunt “Call me Mr Smith”. In Spain, instead of being on first-name terms with patients, the crew is more likely to use less personal forms of address (caballero, señora) and the formal you (Usted). But whichever they opt for, their tone of voice, body language and empathy add nuance to even the greyest word choice. And that’s the common denominator of all professional ambulance workers, wherever they are: in the face of commotion, they’re efficient yet caring and calm.
References
- Davies G, Chesters A. Transport of the trauma patient, Br J Anaesth, 2015;115(1):33-37, https://doi.org/10.1093/bja/aev159
- Abad Esteban F, Abejón Martín R, et al. Manual de Procedimientos de Enfermería SUMMA 112. Consejería de Sanidad, Salud Madrid, 2015. ISBN: 978- 84-695-7511-6 http://www.madrid.org/bvirtual/BVCM017720.pdf
- Barroeta J, Boada N. Los servicios de emergencia y urgencias médicas extra-hospitalarias en España. Mensor, 2011. ISBN: 978-84-615-0990-4 https://www.madrid.es/UnidadesDescentralizadas/Emergencias/Samur-PCivil/Samur/ApartadosSecciones/10_DescargasPublicacionesWebsInteres/Ficheros/Los_SEM_en_Espana.pdf
- NHS Pathways – NHS Digital. NHS Digital. https://digital.nhs.uk/services/nhs-pathways. Accessed 10 March 2022
- Ambulance Quality Indicators Data 2021-22. NHS, https://www.england.nhs.uk/statistics/statistical-work-areas/ambulance-quality-indicators/ambulance-quality-indicators-data-2021-22/. Accessed 10 March 2022
- Actuación ante posibles casos de pacientes infectados por Coronavirus. Manual de Procedimientos, SAMUR Protección Civil, https://www.madrid.es/ficheros/SAMUR/index.html. Accessed 29 April 2022
Image attribution
All photos are my own except the 1970s ambulance (in the public domain) and the LUCAS™ chest compression system, reproduced by kind permission of Stryker.








This is great! Thank you sooo much! Wish a French version existed 🙂